What is Glutamine?
Glutamine is a very popular and widely used amino acid, it is the most abundant amino acid in the body, playing crucial roles in numerous biological processes. Glutamine comprises about 60% of the free amino acid pool within skeletal muscle and 20% of the total circulating amino acids. It is classified as a ‘conditionally essential’ amino acid and being an amino acid, it is a building block of protein. Conditional amino acids are non-essential amino acids that become essential in certain circumstances such as pregnancy or illness. Therefore, glutamine can be synthesised in the body under normal conditions; however, dietary supplementation may become necessary during stress, illness or intense physical activity.
The primary purpose of amino acids is to serve as building blocks for protein. Proteins have many jobs, for example, they help repair body tissues, keep the digestive system working and support the immune system in fighting illness.
Glutamine: Benefits, Uses and Side Effects
Glutamine serves as a primary fuel source for rapidly dividing cells, particularly those of the immune system and intestinal lining. You may have heard about glutamine due to its role in maintaining and repairing the intestinal lining, so it is very often used therapeutically for gut disorders. The intestinal lining consists of cells called enterocytes; they use glutamine as their primary fuel source. It is a valuable amino acid used in a wide range of gut powders on the market.
Glutamine is naturally found in various foods, with the most significant amounts found in animal products due to the high protein content. As glutamine is a necessary part of proteins, in effect, any food containing protein will contain some glutamine.
Food sources include:
- Meat, including beef, pork and poultry.
- Dairy products, including eggs, milk, yogurt and cheese.
- Protein-rich non-animal products, including nuts and tofu.
- Vegetables, including corn and red cabbage.
- Grains, including rice and oats.

Glutamine: What It Is, Benefits & Side Effects
Glutamine has numerous functions within the body.
- Cellular energy source: Glutamine is important for rapidly dividing cells, such as those in the immune system and intestinal lining. Glutamine is an important fuel source for intestinal and immune cells. It helps maintain the barrier between the intestines and the rest of your body, protecting against ‘leaky gut’.
- Nitrogen transport: Glutamine helps transport nitrogen safely to the kidneys for excretion. It is suited to nitrogen transport as it contains two nitrogen atoms per molecule, allowing it to carry nitrogen in a non-toxic form throughout the body safely.
- Protein synthesis: It serves as a building block for various proteins within the body.
- Acid-base balance: It helps maintain a healthy pH and provides a buffer against acidosis.
- Neurotransmitter precursor: Glutamine converts to glutamate, an important excitatory neurotransmitter.
- Immune system support: Fuels immune cells and supports their function.
- Intestinal integrity: Maintains the structure and function of the gut barrier.
Mammalian gut immunity – PubMed
The kidneys play an important role in the conversion of glutamine to glucose through a process called renal gluconeogenesis. This process becomes significant during stress, prolonged fasting and metabolic acidosis. Renal gluconeogenesis from glutamine serves several important functions.
- Acid-base balance: The ammonium ions produced help excrete acid, while this process generates bicarbonate ions, which enter the bloodstream, helping to counteract acidosis.
- Glucose Homeostasis- During times of prolonged fasting, gluconeogenesis can contribute 25-30% of the entire body glucose production. This helps to maintain blood glucose levels.
- Nitrogen disposal- This pathway provides an efficient way to eliminate excess nitrogen while producing glucose at the same time.
- Metabolic adaptation- This process is upregulated during metabolic acidosis, starvation and high protein diets, highlighting the role our kidneys play in this adaptive metabolism.
However, there are considerations to assess if you are taking glutamine as a supplement while you have CKD.
Below is a diagram showing how cells convert glucose into energy through a series of biological processes.
In summary;
Cells convert glucose to energy in a process that’s similar to burning fuel, but much more controlled:
- First breakdown (Glycolysis): Cells split glucose into smaller molecules in the cell’s main compartment. This yields a small amount of energy (ATP) and doesn’t need oxygen.
- Power plant delivery: The breakdown products enter tiny cellular “power plants” called mitochondria.
- Further breakdown (Krebs Cycle): These molecules are broken down completely into carbon dioxide inside mitochondria, releasing electron carriers (like NADH).
- Energy capture (Electron Transport Chain): The electron carriers deliver their electrons to a chain of proteins in the mitochondrial membrane. This creates a kind of “battery charge” across the membrane.
- ATP production: This charge powers a molecular machine (ATP synthase) that makes ATP, the cell’s main energy currency that powers almost everything the cell does.
Think of glucose as a log broken down in steps rather than burned all at once. This controlled breakdown allows cells to grab around 30-32 ATP molecules from each glucose molecule, which they can then use to power cellular activities.

Source: Simplified schematic of glutamine metabolism. Reactions within the box… | Download Scientific Diagram
The Glutaminolysis Pathway in Kidney Disease
Glutaminolysis is the process by which cells break down glutamine to generate energy. Glutaminolysis converts glutamine into the TCA cycle (Citric acid cycle), metabolite alpha-ketoglutarate, through several enzymatic reactions. This metabolic pathway plays a role in inflammation, maladaptive repair, cell survival and proliferation and immune regulation. Glutaminolysis is known for its role in neoplastic cell proliferation. It has also been shown to participate in other pathological and physiological processes such as fibrinogenesis, ischaemic injury, oxidative insult, and aging, as well as in cells with a demand for high energy such as the kidneys. Emerging research is showing, targeting glutaminolysis is a promising therapeutic strategy for reducing kidney disease.
Glutaminolysis is a Potential Therapeutic Target for Kidney Diseases – PMC

Image via Glutaminolysis: A Hallmark of Cancer Metabolism. | Semantic Scholar
The issue with glutamine converting to glucose is that this is not something we want to support in those with CKD; it is something we want to reduce. Ultimately, cells will prefer to use glucose as an energy source, but if they don’t have glucose, the cells may use ketones or glutamine first. Your next question may be, let’s just cut back on glutamine from the diet. This idea is virtually impossible, as you certainly wouldn’t be living on much to survive. The advice here would be, if you have polycystic kidney disease, lupus, diabetic kidney disease or even renal carcinoma, be very careful if you are supplementing with glutamine.
Let’s take a look at why.
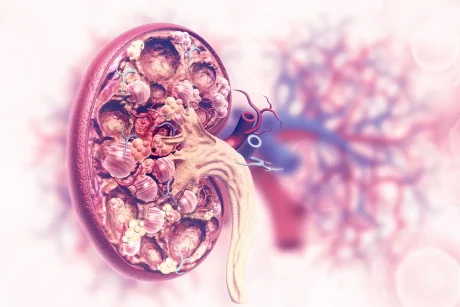
The Connection Between Polycystic Kidney Disease and Glutamine-to-Glucose Conversion: Research and Implications
Polycystic kidney disease (PKD) is a genetic disorder characterised by the growth of numerous fluid-filled cysts in the kidneys, eventually leading to progressive kidney enlargement and dysfunction. Research suggests metabolic alterations, particularly glutamine metabolism and renal gluconeogenesis, play a significant role in disease progression.
In cases of PKD, we want to move clients more towards ketosis, as we want to starve the cells of glucose that can cause cellular turnover. However, if you are taking a lot of glutamine, another process within the cellular cycle can convert glutamine to glucose within the kidneys, keeping this cellular turnover going.
In autosomal dominant polycystic kidney disease (APKD), energy demand is increased due to cyst expansion and cellular proliferation, leading to increased glutamine utilisation. Research shows, cells in APKD undergo metabolic reprogramming, where they favour processes such as aerobic glycolysis as they adapt to conditions associated with cyst growth, mirroring the same behaviour seen in cancer cells, which favour glycolytic pathways over oxidative phosphorylation; known as the Warburg effect. The Warburg effect is seen in cancer cells, where they prefer to metabolise glucose anaerobically rather than aerobically, even when oxygen is available. This metabolic shift allows cancer cells to rapidly produce energy and generate the building blocks needed for rapid cell growth and division.
Defective glucose metabolism in polycystic kidney disease identifies a new therapeutic strategy | Nature Medicine
Pathophysiological Consequences for PKD Patients
This altered glutamine metabolism creates several effects in those with PKD.
- Impaired acid-base handling– The conversion of glucose to glutamine compromises the kidney’s ability to generate bicarbonate, leading to an earlier onset of metabolic acidosis and increased ammonia retention, potentially exacerbating cyst formation.
- Increased promotion of cyst growth- The reprogrammed metabolism directly supports cyst growth through providing the building blocks for cell proliferation, supporting fluid secretion into cyst cavities and creating the microenvironment perfect for cyst expansion.
- Accelerated Disease Progression: Metabolic acidosis resulting from impaired glutamine metabolism can accelerate cyst growth and kidney damage, creating a perfect storm.
Metabolic reprogramming and the role of mitochondria in polycystic kidney disease – ScienceDirect
Implications Seen in Lupus
Glutaminolysis also plays a role in the activation and differentiation of immune cells, especially in cases such as autoimmunity, such as systemic lupus erythematosus (SLE). Research has shown that glutaminolysis significantly influences T cell metabolism and pathogenesis of this disease. This is particularly in respect to the T17 cells, implicated in the inflammatory process associated with lupus. To add, research shows that Th17 cells, characterised by their production of pro-inflammatory cytokines, are highly dependent on glutaminolysis for their differentiation and function. Inhibiting the enzyme glutaminase 1 (GLS1), an enzyme in the glutaminolysis pathway, can reduce Th17 differentiation and reduce symptoms in lupus-prone mouse models. Studies have shown that inhibition of glutaminolysis has a positive impact in reducing pathogenic autoantibody production in lupus models. This suggests an avenue that may help in managing systemic inflammation seen in those with lupus.
Glutaminolysis promotes the function of follicular helper T cells in lupus-prone mice | bioRxiv
Glutaminase 1 Inhibition Reduces Glycolysis and Ameliorates Lupus‐like Disease in MRL/lpr Mice and Experimental Autoimmune Encephalomyelitis
Inhibition of glutaminolysis ameliorates lupus by regulating T and B cell subsets and downregulating the mTOR/P70S6K/4EBP1 and NLRP3/caspase-1/IL-1β pathways in MRL/lpr mice – ScienceDirect
Implications of Diabetic Kidney Disease
Under normal conditions, glutamine can be converted into glucose through gluconeogenesis, which occurs primarily in the liver and kidneys. In DKD, metabolic dysregulation frequently occurs, marked by altered glucose homeostasis. High levels of glucose, common in diabetes, put a significant metabolic burden on the kidneys. This increased burden can impact renal function, leading to metabolic reprogramming that often leads to using glutamine to support energy and gluconeogenic pathways.
The dysregulation of glutamine-to-glucose conversion creates some detrimental effects in the diabetic kidney:
Renal gluconeogenesis contributes to the overall hyperglycemic burden. It creates a vicious cycle where elevated glucose levels further damage renal structures while stimulating glucose production. Some studies suggest that increased renal gluconeogenesis may account for 20-30% of the increased glucose production seen in diabetic patients.
Altered glutamine metabolism contributes to mitochondrial stress in proximal tubular cells. Diabetic patients with kidney disease often develop a type 4 renal tubular acidosis, due to impaired ammonia production from glutamine, further increasing kidney damage.
Understanding the role of dysregulated glutamine-to-glucose conversion and the role of glutaminolysis in kidney pathology and targeting these pathways may become an essential consideration in kidney disease management strategies. The take-home here would be avoiding glutamine in pathologies such as lupus, conditions with a high cell turnover, and PKD and DKD, which would be advised. Those with CKD with a stage of 3 or below also need to be mindful of this. Look at your supplements, what is in them, and use them wisely.
I hope you find this helpful information.