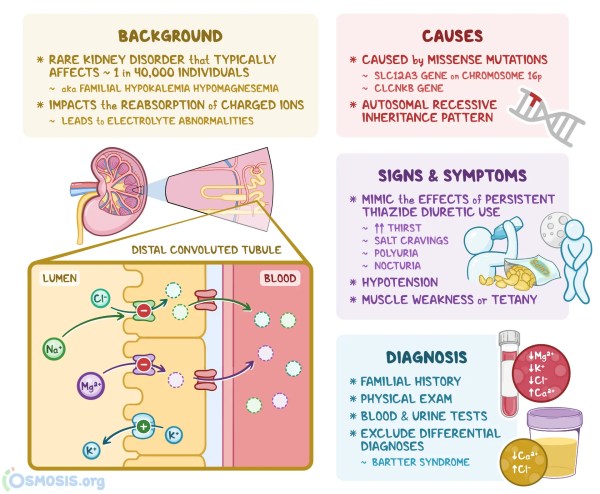
What Is Gitelman Syndrome?
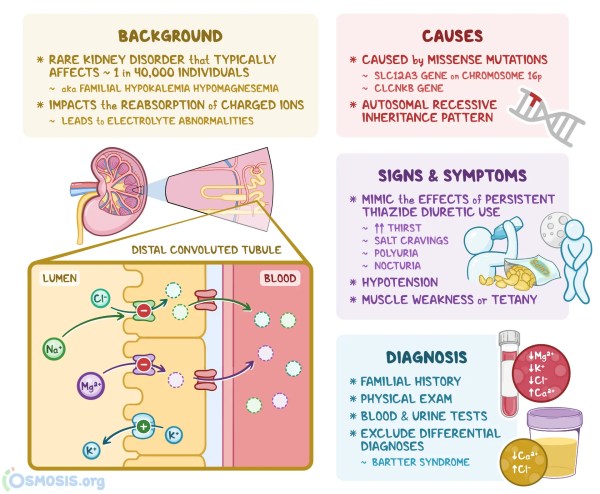
Gitelman syndrome is a rare inherited kidney disorder that causes the body to lose vital salts through urine. Named after Dr. Hiller Gitelman, who identified the condition in 1966, it affects approximately 1 in 40,000 people in the UK. This condition is often considered a milder variant of Bartter syndrome type 3 and typically manifests in late childhood or adulthood, affecting men and women equally.
People with Gitelman syndrome experience electrolyte imbalances that can lead to muscle weakness, fatigue, and other symptoms. While the condition requires lifelong management, most patients can maintain a good quality of life with proper treatment.
Causes of Gitelman Syndrome
Gitelman syndrome is caused by mutations in the SLC12A3 gene, which encodes the thiazide-sensitive sodium-chloride cotransporter (NCC) in the distal convoluted tubule of the kidney. When these genes aren’t functioning properly:
- Salt and potassium are lost in the urine instead of being reabsorbed into the blood
- The movement of ions across the cell membranes in the kidney tubules is disrupted
- The balance of vital electrolytes such as potassium and magnesium is affected
The condition is inherited in an autosomal recessive pattern, meaning a person must inherit two defective copies of the gene (one from each parent) to develop this condition.
The loss of NCC function affects sodium reabsorption and disrupts the balance of other electrolytes. Impaired sodium and chloride absorption leads to increased distal tubular flow, contributing to magnesium wasting.
Gitelman Syndrome – Advances in Chronic Kidney Disease
Symptoms of Gitelman Syndrome
Gitelman syndrome causes a range of symptoms that vary in severity from person to person. Some individuals may be asymptomatic or have mild symptoms discovered only during routine blood tests.
Common Symptoms Include:
- Hypokalaemia (low potassium) causes muscle weakness and cramping. In severe cases, it can lead to cardiac arrhythmias.
- Hypomagnesemia (low magnesium): May cause muscle spasms, tremors, and seizures.
- Hypocalciuria (low calcium in urine): Unlike Bartter Syndrome, patients with Gitelman Syndrome typically show low urinary calcium excretion.
- Fatigue and weakness: Often persistent and may affect daily activities.
- Salt craving: Due to sodium loss, patients often crave salty foods.
- Tingling sensations (paresthesia): Commonly reported in extremities.
- Nocturia: Frequent nighttime urination.
- Joint pain: Can affect mobility and comfort.
- Dizziness: Particularly when standing up quickly.
- Thirst: Increased thirst is common.
- Low blood pressure: May cause light-headedness.
Other Symptoms:
- Metabolic Alkalosis: An imbalance in the body’s acid-base that can cause hypoventilation and confusion.
- Tetany: Involuntary muscle contractions due to electrolyte imbalances.
- Chondrocalcinosis: Calcium deposition in joints (in long-standing cases).
Diagnosis of Gitelman Syndrome
Diagnosing Gitelman syndrome can be challenging due to its similarities with Bartter Syndrome. A comprehensive approach includes:
Clinical Evaluation
- Thorough patient history
- Physical examination
- Assessment of symptoms such as muscle cramps, fatigue, and salt craving
Laboratory Tests
- Serum Electrolytes: Testing for hypokalemia and hypomagnesemia
- Urinary Electrolytes: Assessment of urinary calcium excretion is crucial for distinguishing from Bartter syndrome
- Acid-Base Balance: Evaluation for Metabolic Alkalosis
- Genetic Testing: Identification of mutations in the SLC12A3 gene provides definitive confirmation
Does Gitelman Syndrome Affect Other Parts of the Body?
While Gitelman syndrome primarily affects the kidneys, its symptoms can impact other body systems:
- Muscular system: Weakness and cramps due to electrolyte imbalances
- Cardiovascular system: Potential for arrhythmias with severe hypokalemia
- Nervous system: Tingling sensations and potential cognitive effects with severe imbalances
Importantly, Gitelman syndrome can alter the effects of anesthetics. Patients should always alert their healthcare providers before medical treatment or surgical procedures.
Does Gitelman Syndrome Run in Families?
Gitelman syndrome is a genetic condition that can be inherited from one generation to the next. The inheritance pattern follows autosomal recessive genetics:
- You need to inherit two copies of the mutated gene, one from each parent
- Carriers have one normal copy and one mutated copy of the gene
- Carriers are usually healthy as the normal copy can compensate
- The chance of being a carrier in the general population is less than 1 in 100
When both parents are carriers:
- 25% chance the child will have two normal genes
- 50% chance the child will be a carrier like the parents
- 25% chance the child will have Gitelman syndrome
Treatment of Gitelman Syndrome
Gitelman syndrome treatment focuses on electrolyte repletion and management of symptoms. There is no cure, but the condition can be effectively managed with:
Medication and Supplements
- Oral potassium supplementation: To correct hypokalemia
- Oral magnesium supplementation: Options include magnesium oxide, magnesium chloride, or magnesium glycinate
- Potassium-sparing diuretics: Help retain potassium in the body
- ENaC inhibitors: Used to block the activity of the epithelial sodium channel
- NSAIDs: Reduce renal prostaglandin synthesis, which decreases renal salt wasting
- ACE inhibitors or ARBs: May be used in selected patients to decrease aldosterone production
Dietary Adjustments
- Potassium-rich diet: Foods high in potassium, such as bananas, potatoes, and leafy greens
- Magnesium-rich foods: Including nuts, seeds, and whole grains
- Liberal salt intake: Often recommended, unlike in many other kidney conditions
Ongoing Care
Regular monitoring is crucial for maintaining electrolyte levels, and patients require lifelong treatment and medical supervision. Without proper treatment, potassium and magnesium levels in the blood could become dangerously low, potentially causing heart rhythm problems.
It’s important to note that while Gitelman syndrome affects how well the kidneys function, it doesn’t typically damage their actual structure. Therefore, dialysis or kidney transplantation is rarely required.
Living with Gitelman Syndrome
Most people with Gitelman syndrome can lead normal, active lives with proper management. Key considerations include:
- Regular medical check-ups to monitor electrolyte levels
- Adherence to prescribed supplements and medications
- Awareness of symptoms that may indicate worsening electrolyte imbalances
- Medical ID bracelet or card to alert healthcare providers about the condition
- Genetic counseling for family planning
Natural Interventions for Gitelman Syndrome
While conventional medical treatment remains the cornerstone of Gitelman syndrome management, several complementary natural interventions may help alleviate symptoms and improve quality of life. These approaches should always be implemented under medical supervision and alongside prescribed medications.
Optimised Magnesium Supplementation
The choice of magnesium formulation significantly impacts absorption and effectiveness in Gitelman syndrome:
- Magnesium Glycinate: This highly bioavailable form is bound to the amino acid glycine, which enhances absorption and may cause less gastrointestinal distress than other forms. Research suggests it can be better tolerated at higher doses needed for managing Gitelman syndrome.
- Magnesium Lactate: A slow-release form of magnesium lactate has shown promising results in patient satisfaction surveys. In one study of 28 patients with genetically proven Gitelman syndrome, 89% preferred this treatment regimen over conventional magnesium glycerophosphate, with 68% reporting improved symptom burden and fewer side effects.
- Magnesium Chloride: This form may be particularly beneficial for Gitelman syndrome patients as it provides both magnesium and chloride, which are depleted in this condition.
Combination Supplements
Emerging research suggests potential benefits from combining magnesium with other nutrients:
- Magnesium with L-carnitine: This combination has shown synergistic effects in studies of other conditions involving electrolyte imbalances. L-carnitine plays a key role in cellular energy production and may help improve fatigue symptoms common in Gitelman syndrome.
- Potassium and Magnesium Co-supplementation: The close metabolic relationship between these electrolytes means magnesium restoration alone can sometimes improve potassium levels. Research indicates that “when potassium and magnesium depletion coexist, magnesium restoration alone is sufficient to correct hypokalemia.”
Mind-Body Interventions
Several mind-body practices show promise for supporting kidney health and managing symptoms associated with Gitelman syndrome:
Acupuncture
Acupuncture has demonstrated benefits for kidney function and electrolyte balance:
- Blood Pressure Regulation: Studies show acupuncture can help regulate blood pressure by affecting the renin-angiotensin-aldosterone system, which maintains fluid and electrolyte balance.
- Sympathetic Nervous System Modulation: Research indicates acupuncture may help regulate the autonomic nervous system, potentially improving kidney blood flow and function.
Meditation and Mindfulness Practices
Regular meditation may provide several benefits for people with kidney conditions like Gitelman syndrome:
- Blood Pressure Reduction: A study of African-American males with chronic kidney disease found that mindfulness meditation significantly reduced blood pressure and sympathetic nerve activity compared to controls.
- Stress Management: Since stress can exacerbate electrolyte imbalances, meditation techniques that reduce stress may indirectly help stabilise electrolytes.
- Quality of Life Improvement: Research has shown that guided meditation (Yoganidra) improves quality of life measurements in patients with kidney disease, including physical well-being and happiness.
Hydration Strategies
Proper hydration is crucial for people with Gitelman syndrome, but requires a strategic approach:
- Structured Fluid Intake: Rather than simply increasing fluid volume, spreading hydration throughout the day can help maintain more consistent electrolyte levels.
- Electrolyte-Infused Hydration: Consuming beverages with balanced electrolytes (particularly sodium, potassium, and magnesium) may be more beneficial than plain water.
- Monitoring Hydration Status: Learning to recognise personal hydration needs based on urine colour, thirst, and energy levels can help avoid dehydration, which can worsen electrolyte imbalances.
Salt Loading
Unlike many kidney conditions that require salt restriction, Gitelman syndrome often benefits from increased salt intake:
- Sodium Chloride Supplementation: People with Gitelman syndrome are encouraged to increase salt intake, particularly sodium chloride (table salt). One clinical approach involves using slow sodium tablets (Slow Sodium® 600 mg) administered in divided doses.
- Salt Craving Response: Patients are encouraged to listen to their body’s salt cravings, as this can be a natural signal that more salt is needed to help balance electrolytes.
- Individualised Approach: The optimal amount of salt varies by individual and should be determined with medical supervision based on blood pressure, symptoms, and electrolyte levels.
Dietary Considerations
Beyond general dietary guidelines for Gitelman syndrome, some specific nutritional approaches may help:
- Potassium-Rich Foods: Strategically incorporating high-potassium foods like bananas, potatoes, and leafy greens can support dietary potassium intake.
- Magnesium-Rich Foods: Regularly consuming foods high in magnesium, such as nuts, seeds, whole grains, and dark chocolate, may complement supplementation.
- Anti-Inflammatory Diet: Since chronic electrolyte imbalances can contribute to inflammation, an anti-inflammatory diet rich in omega-3 fatty acids, antioxidants, and whole foods may provide additional benefits.
Important Considerations
Several key points should be kept in mind when considering natural interventions:
- Medical Supervision is Essential: Due to the complex nature of electrolyte management in Gitelman syndrome, all natural interventions should be implemented under close medical supervision.
- Individualised Approach: Response to interventions varies significantly between individuals with Gitelman syndrome, even those with identical genetic mutations.
- Adjunctive Role: Natural interventions should complement, not replace, conventional treatment with electrolyte supplementation and medications.
- Regular Monitoring: Frequent electrolyte testing is necessary when implementing any new intervention to ensure safety and efficacy.
- Research Limitations: Evidence supporting many natural interventions specifically for Gitelman syndrome is limited, with most studies being small case series rather than large clinical trials.
Key Takeaways
- Gitelman syndrome is a rare genetic kidney disorder affecting approximately 1 in 40,000 people
- It causes loss of essential salts through urine due to mutations in the SLC12A3 gene
- Primary symptoms include low potassium, low magnesium, fatigue, and muscle weakness
- Diagnosis involves blood and urine tests, with genetic testing providing confirmation
- Conventional treatment focuses on electrolyte replacement and symptom management
- Natural interventions that may complement medical treatment include:
- Specialised magnesium formulations (glycinate, lactate, or chloride forms)
- Mind-body practices like meditation and acupuncture
- Strategic salt loading and structured hydration
- Combination supplements like magnesium with L-carnitine
- All natural interventions should be implemented under medical supervision
- With an integrative approach combining conventional and complementary treatments, most patients can maintain a good quality of life.
For more information about Gitelman syndrome and other kidney conditions, consult with a nephrologist or visit trusted resources like Kidney Care UK or the National Organisation for Rare Disorders (NORD).