What Are GLP-1 and GLP-2 Peptides?
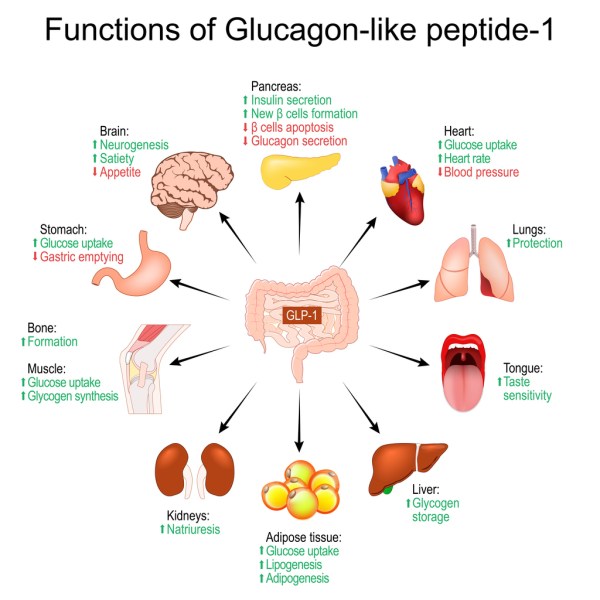
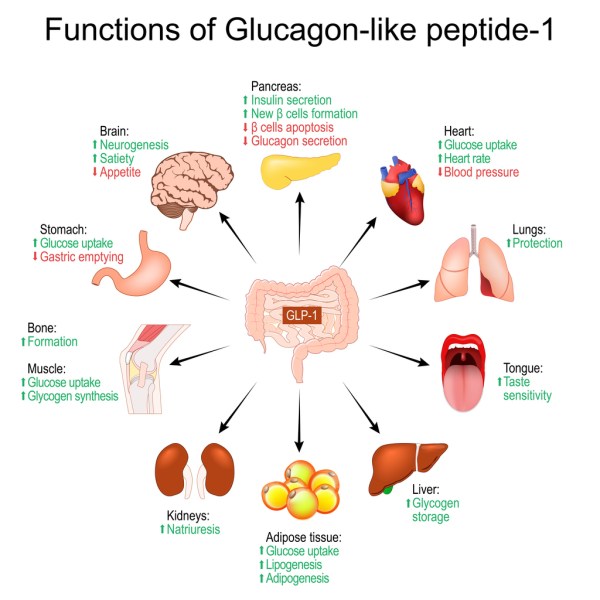
GLP-1 (Glucagon-Like Peptide-1) and GLP-2 (Glucagon-Like Peptide-2) are naturally occurring hormones classified as incretins produced in the gut in response to food intake. They are vital in regulating glucose metabolism, appetite, and various digestive processes. Both peptides have become targets for therapeutic interventions due to their beneficial effects on metabolic health, weight management, and digestive disorders.
GLP-1 Peptides: Role and Therapeutic Uses
GLP-1 is primarily involved in glucose metabolism. Upon release, it enhances insulin secretion in response to elevated blood sugar levels, slows gastric emptying, and promotes a feeling of fullness (satiety). It also inhibits glucagon release, preventing excessive glucose production in the liver. These effects make GLP-1 a powerful tool in managing type 2 diabetes and obesity.
Key Medications:
- Exenatide (Byetta)
- Liraglutide (Victoza, Saxenda)
- Semaglutide (Ozempic, Wegovy)
- Tirzepatide (Mounjaro)
GLP-1 receptor agonists (GLP-1 RAs) are widely used to:
- Improve glycemic control in type 2 diabetes.
- Support weight loss by reducing appetite and caloric intake.
- Enhance cardiovascular outcomes in diabetic patients by lowering the risk of major cardiovascular events.
Their physiological and pharmacological properties vary depending on which receptors these medications activate. Earlier drugs like liraglutide, liraglutide, and tirzepatide target these receptors differently. For example, tirzepatide is sometimes called a “triple GLP” because it hits three receptors. Each drug has different effects—some people respond better to one drug, while others may experience side effects like bloating or nausea, depending on their genetic makeup and receptor density.
These medications not only target the pancreas but also affect bile production, motility, and many other systems in the body. They even influence intestinal cell junctions.
Tirzepatide
Mounjaro is a medication developed by Eli Lilly. Its active ingredient is Tirzepatide, a novel peptide that targets two key incretin receptors in the body: GLP-1 (Glucagon-Like Peptide-1) and GIP (Glucose-Dependent Insulinotropic Polypeptide). This dual-action mechanism makes Mounjaro a groundbreaking treatment for both type 2 diabetes and obesity.
How Does Tirzepatide Work?
Tirzepatide is unique because it mimics the effects of both GLP-1 and GIP (Gastric inhibitory polypeptide). These two incretin hormones are naturally released after eating to regulate blood sugar and fat metabolism. By activating both receptors, tirzepatide enhances insulin release, decreases glucagon production, slows gastric emptying, and increases satiety (the feeling of fullness), making it highly effective for:
- Lowering blood glucose levels in people with type 2 diabetes.
- Promoting weight loss by reducing appetite and food intake.
Therapeutic Benefits of Tirzepatide
- Type 2 Diabetes Management:
- Tirzepatide helps improve glycemic control by increasing insulin secretion and reducing glucagon levels, both of which help to lower blood sugar levels after meals. In clinical trials, tirzepatide has shown superior glucose-lowering effects compared to traditional GLP-1 receptor agonists like semaglutide.
- It also has beneficial effects on HbA1c (a marker of long-term blood sugar levels), with many patients achieving significant reductions in their HbA1c levels.
- Weight Loss:
- One of the most remarkable effects of tirzepatide is its ability to promote significant weight loss. This makes Mounjaro a valuable option for people with obesity, even those without type 2 diabetes. Clinical studies show that patients treated with Mounjaro experienced greater weight loss compared to those on existing GLP-1 medications.
- In some studies, patients lost up to 20% of their body weight, a result comparable to bariatric surgery in certain cases.
- Cardiovascular Benefits:
- Like other incretin-based therapies, Mounjaro has shown promise in reducing cardiovascular risk. By improving glycemic control and promoting weight loss, tirzepatide may help lower the risk of heart attacks, strokes, and other cardiovascular events in high-risk patients.
- Potential in Treating Other Conditions:
- Tirzepatide’s dual mechanism offers promise for treating other conditions beyond diabetes and obesity. Researchers are investigating its use in managing fatty liver disease (NAFLD), chronic kidney disease (CKD), and potentially even Alzheimer’s disease, due to its effects on metabolism and inflammation.
Tirzepatide vs. Other GLP-1 Medications
While both tirzepatide (Mounjaro) and other GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) target the GLP-1 receptor, tirzepatide offers additional benefits by also targeting the GIP receptor. This dual action enhances its efficacy, particularly in terms of weight loss and glycemic control.
In trials, tirzepatide has shown to be more effective than GLP-1-only medications in both lowering blood sugar and promoting weight loss. It is often referred to as a “triple incretin” because it impacts insulin, glucagon, and the body’s fat metabolism in a highly integrated manner.
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2821080
Side Effects and Considerations
Common side effects of tirzepatide include:
- Nausea, vomiting, and diarrhea, especially when first starting the medication.
- Delayed gastric emptying, which can lead to feelings of fullness or bloating.
- In rare cases, more severe side effects such as pancreatitis or gallbladder issues may occur.
Some patients may also experience a condition called “Ozempic face” or “Mounjaro face,” where rapid weight loss results in a loss of facial fat, giving a gaunt appearance. This can be managed through careful dose adjustments and adjunct therapies, including exercise, a proper diet and co use of other peptides and things like collagen.
Future Applications of Tirzepatide
While currently approved for type 2 diabetes and weight management, tirzepatide is being studied for its potential in treating a wide range of metabolic and inflammatory conditions. Its ability to modulate both GLP-1 and GIP receptors opens the door to possible applications in non-alcoholic steatohepatitis (NASH), chronic kidney disease (CKD), and even neurodegenerative diseases due to its impact on metabolic pathways and inflammation.
The Use of GLP-1 Receptor Agonists in Chronic Kidney Disease (CKD)
Chronic Kidney Disease (CKD) is a progressive condition characterized by the gradual loss of kidney function, often due to diabetes, hypertension, or other metabolic disorders. As the kidneys lose their ability to filter waste from the blood, patients face complications like proteinuria, fluid imbalances, and, ultimately, kidney failure. In recent years, GLP-1 receptor agonists have emerged as promising treatments to help slow the progression of CKD, especially in patients with type 2 diabetes.
These medications have shown promise in managing chronic kidney disease (CKD). While reducing glucose levels and body weight helps, they also improve kidney health by directly affecting receptors in the kidneys. They lessen the tension that leads to fibrosis and improve endothelial permeability, which is essential for kidney filtration. They also reduce sympathetic overstimulation, a factor that exacerbates kidney disease.
Moreover, they reduce inflammation in the kidneys by modulating immune responses, particularly in conditions like interstitial nephritis. These medications also affect fibrosis, reducing the likelihood of tissue sclerosis, which is crucial for preventing CKD from progressing to later stages.
How GLP-1 Receptor Agonists Work in CKD
GLP-1 receptors are found not only in the pancreas but also in the kidneys, cardiovascular system, and other tissues, which enables these drugs to exert protective effects beyond glycemic control.
Renal Protective Effects of GLP-1 Agonists
- Reduction in Proteinuria
- Proteinuria, or the presence of excess protein in the urine, is an early sign of kidney damage. Studies have shown that GLP-1 receptor agonists can reduce proteinuria, which may help slow the progression of CKD.
- By improving insulin sensitivity and reducing blood sugar levels, GLP-1 agonists decrease the stress on the kidneys caused by high glucose levels. This reduces glomerular hyperfiltration (increased pressure in the kidney’s filtering units), which is a key driver of kidney damage in diabetic patients.
- Blood Pressure Stabilization
- High blood pressure is a major contributor to the progression of CKD. GLP-1 receptor agonists help lower blood pressure by promoting vasodilation (the widening of blood vessels) and reducing the overall workload on the heart and kidneys. This effect can be particularly beneficial for CKD patients, as reducing blood pressure helps slow the decline of kidney function.
- Reduction in Inflammation and Fibrosis
- Chronic inflammation is a hallmark of CKD, leading to fibrosis (scarring) and loss of kidney function over time. GLP-1 receptor agonists have demonstrated anti-inflammatory effects that help reduce oxidative stress and inflammation in the kidneys.
- By inhibiting the processes that lead to fibrosis, GLP-1 drugs help protect the kidney’s structural integrity. This is critical in preventing the progression of CKD from early stages to end-stage kidney disease (ESKD), which often requires dialysis or kidney transplantation.
- Impact on Cardiovascular Risk
- Cardiovascular disease is a leading cause of death in patients with CKD. GLP-1 receptor agonists have well-established cardiovascular benefits, such as reducing the risk of heart attacks, strokes, and heart failure. For CKD patients, managing cardiovascular risk is crucial, as impaired kidney function and cardiovascular issues often go hand in hand.
- The reduction in blood sugar, body weight, and blood pressure that comes with GLP-1 use also lowers the overall cardiovascular burden, thereby helping to protect kidney function in the long term.
https://link.springer.com/article/10.1007/s12020-024-03757-9
Evidence from Clinical Trials
Several clinical trials have highlighted the benefits of GLP-1 receptor agonists in people with CKD, particularly those with diabetic kidney disease (diabetic nephropathy), which is a leading cause of CKD. The LEADER trial, which evaluated the effects of liraglutide (Victoza) in type 2 diabetes patients, showed that the drug significantly reduced the risk of kidney-related adverse events, including new-onset persistent macroalbuminuria (a marker of kidney damage).
Similarly, the SUSTAIN-6 trial, focusing on semaglutide (Ozempic), demonstrated significant reductions in the progression of kidney disease, especially in reducing albuminuria and slowing the decline in glomerular filtration rate (GFR), which is a key measure of kidney function.
Tirzepatide (Mounjaro) also shows potential for kidney protection, though long-term studies are ongoing. The dual action on both GLP-1 and GIP receptors offers enhanced metabolic benefits, and it’s expected to have more substantial renal protective effects compared to traditional GLP-1 therapies.
https://www.nature.com/articles/s41467-024-50199
https://www.nejm.org/doi/full/10.1056/NEJMoa2403347
https://pubmed.ncbi.nlm.nih.gov/38411162/
https://cardiab.biomedcentral.com/articles/10.1186/s12933-023-01793-9
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2789684
Mechanisms of Action in CKD
- Glomerular Protection
- GLP-1 receptor agonists reduce the pressure within the glomeruli, the kidney’s filtration units, by lowering blood pressure and improving insulin sensitivity. This glomerular protection is vital for preventing kidney damage, especially in diabetic patients.
- Reduction of Oxidative Stress
- Oxidative stress plays a major role in kidney damage. GLP-1 agonists reduce oxidative stress in the kidneys by increasing the production of antioxidant enzymes and reducing the formation of reactive oxygen species (ROS), which can damage kidney cells.
- Modulation of Sympathetic Nervous System Activity
- Overactivity of the sympathetic nervous system contributes to the progression of CKD. GLP-1 agonists reduce sympathetic nervous system activity, helping to lower blood pressure and protect the kidneys from further damage.
Who Benefits the Most from GLP-1 Agonist Therapy in CKD?
- Diabetic CKD Patients: GLP-1 receptor agonists are particularly effective in patients with type 2 diabetes and CKD, where their ability to improve glycemic control, reduce inflammation, and protect the kidneys has been well-documented.
- Non-Diabetic CKD Patients: Although most studies have focused on diabetic CKD, there is emerging interest in using GLP-1 receptor agonists for non-diabetic CKD patients. The anti-inflammatory, anti-fibrotic, and cardiovascular benefits could make these drugs a useful treatment for other forms of CKD as well, such as hypertensive nephropathy.
Current Limitations and Ongoing Research
While GLP-1 receptor agonists have shown great promise in managing CKD, there are still some limitations:
- Renal dosing considerations: In patients with advanced CKD (eGFR < 30 mL/min/1.73 m²), using some GLP-1 receptor agonists requires careful consideration, as their clearance may be affected by reduced kidney function.
- Long-term outcomes: More research is needed to determine the long-term renal benefits of GLP-1 agonists in non-diabetic CKD patients and to explore their full potential in preserving kidney function in diverse patient populations.
Ongoing studies are expected to provide more data on:
- The effects of GLP-1 receptor agonists in reducing the progression of CKD in non-diabetic populations.
- Combination therapies: The use of GLP-1 agonists alongside other kidney-protective medications, such as SGLT-2 inhibitors, is being explored for their synergistic benefits in managing CKD.
GLP-1 receptor agonists offer a promising avenue for slowing the progression of CKD, particularly in diabetic patients. By addressing key risk factors such as hyperglycemia, hypertension, and inflammation, these drugs not only help preserve kidney function but also reduce the risk of cardiovascular events in CKD patients. As more research unfolds, GLP-1 receptor agonists may become a standard part of CKD management, offering hope for patients with this progressive and often life-threatening condition.
Other Off-Label Uses of GLP-1 Receptor Agonists
1. Cardiovascular Disease
GLP-1 receptor agonists have demonstrated significant cardiovascular benefits in clinical trials, particularly in people with type 2 diabetes. Off-label, these medications are being considered for:
- Reducing cardiovascular risk in non-diabetic individuals: GLP-1 drugs may help lower the risk of heart attacks and strokes by improving endothelial function, reducing inflammation, and aiding in weight loss.
- Heart failure and atherosclerosis: Emerging research suggests that GLP-1 therapy may improve heart function and reduce the progression of atherosclerosis, even in those without diabetes.
2. Non-Alcoholic Fatty Liver Disease (NAFLD) and Non-Alcoholic Steatohepatitis (NASH)
NAFLD and NASH are metabolic liver conditions associated with obesity and insulin resistance. Off-label use of GLP-1 receptor agonists has shown promising results in:
- Reducing liver fat content: Studies suggest that GLP-1 agonists may help reverse fatty liver by improving insulin sensitivity and promoting weight loss.
- Lowering liver inflammation and fibrosis: GLP-1 drugs may reduce the inflammation and fibrosis associated with NASH, a serious liver condition that can lead to cirrhosis and liver failure.
3. Alzheimer’s Disease and Neurodegenerative Disorders
There is growing interest in the potential of GLP-1 receptor agonists as treatments for neurodegenerative diseases such as Alzheimer’s and Parkinson’s. The off-label focus here is on:
- Neuroprotection and cognitive enhancemente=”font-weight: 400;”>: GLP-1 receptors are present in the brain, and early studies suggest that these medications may enhance neuroplasticity, reduce neuroinflammation, and improve cognitive function. GLP-1 analogs may help slow the progression of Alzheimer’s by reducing the accumulation of amyloid plaques and tau proteins.
- Potential treatment for Parkinson’s disease: Preclinical studies show that GLP-1 agonists may help reduce dopaminergic neuron loss and protect against motor function decline.
4. Polycystic Ovary Syndrome (PCOS)
PCOS is a common endocrine disorder that often leads to insulin resistance, obesity, and metabolic issues. Off-label use of GLP-1 agonists has shown potential for:
- Improving insulin sensitivity: GLP-1 receptor agonists can help women with PCOS manage insulin resistance, a key component of the syndrome.
- Aiding weight loss and improving reproductive function: By promoting weight loss and improving metabolic parameters, GLP-1 drugs may help regulate menstrual cycles and improve fertility in women with PCOS.
5. Weight Loss in Non-Diabetic Patients
While GLP-1 receptor agonists are approved for weight management in people with type 2 diabetes or obesity, off-label use for general weight loss in non-diabetic individuals is becoming increasingly popular. GLP-1 drugs help by:
- Suppressing appetite: By modulating the brain’s appetite centers, these medications reduce food intake, leading to significant weight loss, even in non-diabetic individuals.
- Improving metabolic health: Beyond weight loss, GLP-1 drugs help improve metabolic markers such as cholesterol levels and insulin sensitivity.
6. Addiction Treatment
Another emerging area for off-label use of GLP-1 receptor agonists is in the treatment of substance abuse disorders, including:
- Nicotine and alcohol addiction: Early research suggests that GLP-1 agonists may reduce the reinforcing effects of addictive substances like nicotine and alcohol, possibly by influencing dopamine signaling pathways in the brain.
- Food addiction: Given GLP-1’s effects on appetite control, there’s interest in its potential to treat binge-eating and food addiction.

https://www.nature.com/articles/nrendo.2012.140
What’s Coming Down the Scientific Pipeline?
As research on GLP-1 receptor agonists continues, there are several exciting developments on the horizon that could expand their therapeutic use.
1. Dual and Triple Agonists
Following the success of tirzepatide (Mounjaro), which targets both GLP-1 and GIP receptors, the next generation of medications will likely include &amp;amp;amp;amp;amp;amp;amp;amp;amp;lt;/span>dual and triple agonists that activate additional pathways, such as glucagon receptors, for even greater metabolic benefits. These agonists are designed to:
- Optimize glucose and fat metabolism: By targeting multiple receptors, these therapies may improve glycemic control, enhance fat burning, and accelerate weight loss more effectively than current GLP-1 therapies.
- Treat metabolic liver disease: Early research on triple agonists suggests potential benefits for liver conditions like NASH and NAFLD, further improving insulin sensitivity and liver health.
2. Oral GLP-1 Agonists
While current GLP-1 receptor agonists are typically administered via injection, research is underway to develop oral formulations. This would increase accessibility and convenience for patients, especially those who are resistant to injectable treatments. Early studies on oral semaglutide (Rybelsus) show promise for managing diabetes and weight loss.
3. Inflammation and Autoimmune Conditions
GLP-1’s role in modulating the immune system is an area of intense interest. Researchers are exploring its potential in treating chronic inflammatory and autoimmune diseases, such as:
- Rheumatoid arthritis
- Crohn’s disease and ulcerative colitis
- Psoriasis
The anti-inflammatory effects of GLP-1 agonists may help reduce immune system overactivity and tissue damage in these conditions.
4. Cancer Research
Preliminary studies suggest that GLP-1 receptor agonists may have potential anti-cancer properties by:
- Reducing tumor growth: Animal studies indicate that GLP-1 agonists may slow the growth of certain cancers, including breast and colorectal cancer.
- Improving chemotherapy outcomes: There’s also interest in using GLP-1 analogs to enhance the efficacy of chemotherapy while reducing its side effects, particularly in metabolic complications associated with cancer.
5. Gut Microbiome and Longevity
There’s emerging research on how GLP-1 receptor agonists may influence the gut microbiome, improving gut health and potentially influencing longevity:
- Modulating gut bacteria: GLP-1 drugs may help create a healthier balance of gut bacteria, which is linked to better metabolic health and lower inflammation.
- Longevity research: As GLP-1 agonists improve key markers of metabolic and cardiovascular health, some researchers are investigating their role in extending health span and lifespan by preventing age-related diseases.
Final Thoughts
GLP-1 receptor agonists have already proven to be revolutionary for managing type 2 diabetes and obesity, but ongoing research and off-label uses show that their potential goes far beyond these applications. From neurodegenerative diseases to chronic kidney disease, cardiovascular health, and even addiction treatment, GLP-1 receptor agonists are poised to become critical tools in treating a wide array of conditions in the near future. But, they have side effects and, in my opinion, should never be used as a monotherapy (a stand-alone therapy). We always need to ensure that one’s diet and lifestyle are optimised towards kidney health first before we think about adding these types of medications. Also, in speaking to many doctors who are using and prescribing these medications, using them with other peptides to reduce side effects and preserve muscle mass is paramount.
As always, please talk to your healthcare provider before starting any new medications.
Let us know your thoughts by heading to our Facebook page.