Oxytocin is often called the ‘love hormone’ because of its well-known role in childbirth, breastfeeding, and emotional bonding. But emerging research reveals this remarkable hormone does far more than foster maternal connection. Scientists are now discovering that oxytocin plays a crucial role in kidney function and may offer significant protective benefits for people with chronic kidney disease (CKD).
Chronic kidney disease affects approximately 37 million Americans and hundreds of millions worldwide, progressively damaging the kidneys’ ability to filter waste, regulate blood pressure, and maintain proper fluid balance. While conventional treatments focus on managing symptoms and slowing progression through medications and dietary modifications, researchers are uncovering novel biological pathways that may help protect kidney function and oxytocin appears to be a key player in several of these protective mechanisms.
This comprehensive guide explores the fascinating connection between oxytocin and kidney health, revealing how this hormone influences renal function, reduces dangerous inflammation, and may help prevent kidney damage through surprising pathways including your gut microbiome, vagus nerve activation, and social connections. Understanding these connections may open new doors for complementary approaches to kidney disease management that work synergistically alongside conventional medical care.
What Is Oxytocin and Why Does It Matter for Kidney Health?
Oxytocin is a hormone and neuropeptide produced in the hypothalamus and released by the posterior pituitary gland. While best known for triggering uterine contractions during labour and stimulating milk release during breastfeeding, oxytocin acts as both a hormone and a neuromodulator, affecting multiple body systems simultaneously through complex signaling pathways.
What makes oxytocin particularly interesting for kidney health is its presence throughout the body, including in kidney tissue itself. Oxytocin receptors have been identified in various kidney structures, particularly in the juxtaglomerular apparatus, which regulates blood pressure and filtration. This discovery suggests this hormone directly influences renal function rather than working solely through systemic effects, opening entirely new research directions for therapeutic interventions.
Oxytocin’s Wide-Ranging Effects in Your Body
Beyond reproduction and bonding, oxytocin influences numerous physiological processes that directly and indirectly affect kidney function and overall health:
• Brain and emotional regulation: Oxytocin receptors are concentrated in the hippocampus, amygdala, and nucleus accumbens brain regions that control emotion, reward processing, social behavior, and stress responses. This neural activity directly impacts systemic inflammation and cardiovascular function, both of which are critical for kidney health.
• Metabolic function: Reduces appetite, increases fat oxidation, improves insulin sensitivity, and helps regulate lipid metabolism. These metabolic effects are particularly important for kidney disease patients, who often struggle with metabolic syndrome and insulin resistance.
• Cardiovascular health: By promoting parasympathetic nervous system activation, oxytocin helps lower blood pressure, reduce heart rate, and decrease cardiovascular stress all factors that significantly impact long-term kidney function.
• Anti-inflammatory effects: Reduces oxidative stress and systemic inflammation, protecting multiple organ systems including the kidneys from inflammatory damage that drives disease progression.
• Bone metabolism: Supports bone formation and density by regulating osteoblast differentiation and inhibiting osteoclast activity important for CKD patients who face increased fracture risk due to mineral bone disease.
• Sleep regulation: By activating the ‘rest and digest’ parasympathetic state, oxytocin promotes better sleep quality and recovery, which are essential for healing and maintaining kidney function.
These diverse effects demonstrate that oxytocin functions as a master regulator linking emotional well-being, metabolic health, and organ function, including kidney health.
The Surprising Gut-Kidney-Oxytocin Connection
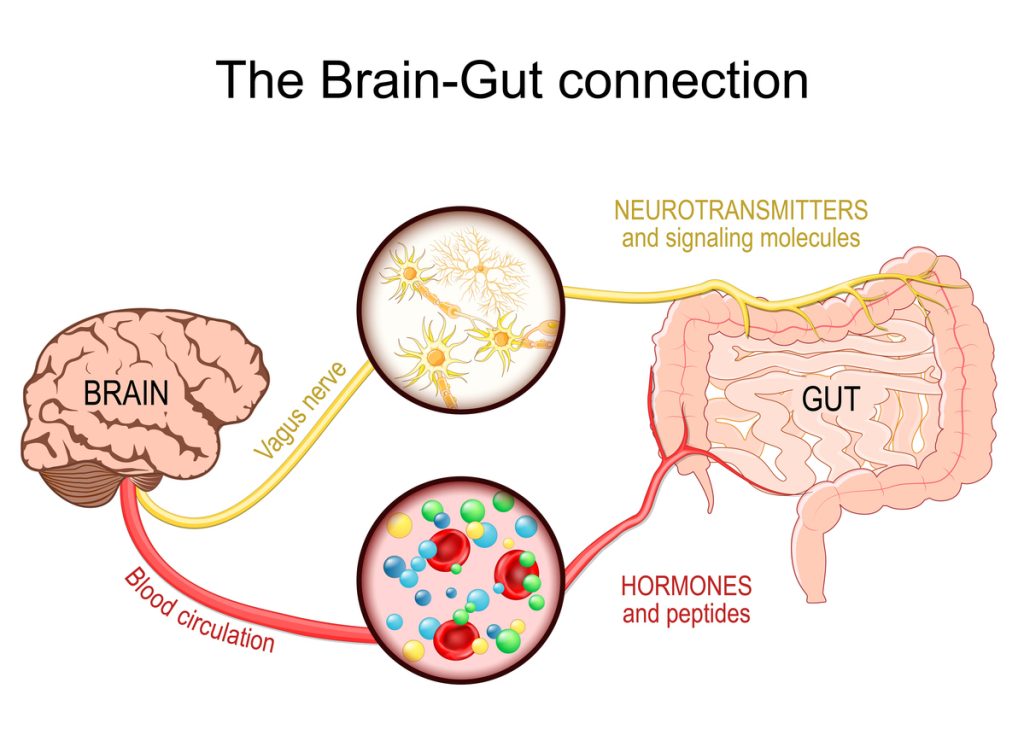
One of the most exciting discoveries is that oxytocin isn’t only produced in the brain, it’s also synthesized and released in your gastrointestinal tract. This finding creates a fascinating three-way connection between your gut microbiome, oxytocin levels, and kidney health that challenges traditional understanding of how these systems interact.

How Gut Bacteria Influence Oxytocin Production
The human gut contains trillions of bacteria that profoundly influence health through multiple mechanisms. Research has revealed that certain beneficial bacteria, particularly Lactobacillus reuteri, can directly stimulate oxytocin production in the intestine through a fascinating cascade:
• L. reuteri and other probiotic bacteria colonize the intestinal lining and interact with specialized hormone-producing cells
• These bacteria stimulate enteroendocrine cells scattered throughout the intestinal wall
• The stimulated cells release secretin, an important gut hormone that regulates digestive processes
• Secretin triggers enterocytes (intestinal cells) to produce and release oxytocin into circulation
• This gut-produced oxytocin enters the bloodstream and affects multiple organ systems, including the kidneys
This gut-brain-kidney axis represents a powerful new mechanism for understanding how microbiome health influences kidney function. A balanced, diverse microbiome supports oxytocin production, which in turn contributes to healthier metabolism, reduced systemic inflammation, improved vascular function, and enhanced kidney protection.
For people with chronic kidney disease, this connection is particularly important because CKD itself disrupts the gut microbiome through uremic toxin accumulation, dietary restrictions, and frequent antibiotic use. Supporting gut health through targeted probiotics, prebiotics, and appropriate dietary choices may help restore healthy oxytocin signaling and provide kidney-protective benefits.

Image via Oxytocin and the microbiome – ScienceDirect
The Vagus Nerve: Your Body’s Oxytocin Highway
The vagus nerve serves as the primary communication pathway connecting your brain, gut, heart, and kidneys. This remarkable nerve operates like a sophisticated two-way highway, constantly transmitting information about your body’s physiological and emotional state between the central nervous system and peripheral organs.
Oxytocin and the vagus nerve work together in a positive feedback loop that’s crucial for health. The vagus nerve activates the parasympathetic nervous system your ‘rest, digest, and heal’ mode which creates the safe, calm conditions where oxytocin is most readily released. In turn, oxytocin enhances vagal tone, deepening relaxation, improving heart rate variability, and supporting kidney function through improved blood flow and reduced inflammatory responses.
For kidney health specifically, vagal activation is particularly important because it:
• Reduces sympathetic nervous system overactivity, which damages kidneys over time through chronic vasoconstriction
• Lowers blood pressure and improves vascular function throughout the cardiovascular system
• Decreases inflammatory cytokine production that drives kidney tissue damage
• Enhances kidney perfusion and glomerular filtration rate
• Improves the body’s stress resilience and recovery capacity
Natural Ways to Boost Oxytocin for Kidney Health
While no specific foods directly increase oxytocin levels, you can support your body’s natural oxytocin production through lifestyle practices that activate the vagus nerve, promote gut health, and create the physiological conditions for optimal oxytocin release:
• Deep, slow diaphragmatic breathing exercises such as 4-7-8 breathing or box breathing
• Physical touch, including massage, hugging, and therapeutic bodywork
• Meaningful social bonding and authentic connections with loved ones
• Sexual intimacy and physical affection with partners
• Genuine laughter and joyful experiences
• Sustained eye contact during conversations with trusted people
• Meditation, mindfulness practices, and loving-kindness meditation
• Music, singing, chanting, and dancing, especially in groups
• Anti-inflammatory, gut-friendly diet rich in prebiotic and probiotic foods like fermented vegetables, yogurt, and kefir
• Regular moderate exercise, particularly activities done with others
• Quality sleep in a safe, comfortable environment
• Pet ownership and animal-assisted therapy
Factors That Decrease Oxytocin Production
Understanding what depletes oxytocin is equally important for protecting kidney health. Several factors can disrupt healthy oxytocin levels and should be addressed when possible:
• Chronic stress and persistently elevated cortisol levels
• Social isolation, loneliness, and lack of meaningful connection
• Depression, anxiety disorders, and mood dysregulation
• Childhood trauma, neglect, and attachment disruptions
• Low estrogen levels, particularly post-menopause
• Chronic inflammation and autoimmune conditions
How Chronic Kidney Disease Affects Oxytocin Levels
Chronic kidney disease creates a problematic bidirectional cycle involving oxytocin dysregulation. CKD is characterized by both systemic and localized renal inflammation, driven by uremic toxin accumulation, oxidative stress, and immune system activation. Elevated pro-inflammatory cytokines such as IL-6, TNF-alpha, and IL-1beta trigger neuroinflammatory responses that directly affect the hypothalamus, where oxytocin is produced and regulated.
This inflammatory cascade can decrease both oxytocin production and receptor sensitivity, which is particularly problematic because oxytocin itself has protective effects against the very inflammation and metabolic dysregulation that drive kidney disease progression. This creates a vicious cycle where kidney disease reduces oxytocin, and low oxytocin allows more kidney damage to occur. Breaking this cycle through interventions that support oxytocin production may offer significant benefits for CKD patients beyond what conventional treatments alone can provide.
Oxytocin’s Protective Effects on Kidney Function
Research has identified several distinct mechanisms through which oxytocin may protect kidney health and potentially slow CKD progression. While much of this research comes from animal models and small human studies, the findings are compelling enough to warrant further investigation and clinical trials.
Oxytocin Regulates Kidney Blood Flow and Filtration
Oxytocin receptors exist within kidney tissue, particularly concentrated in the juxtaglomerular apparatus a specialized structure that regulates blood pressure and kidney filtration. Research suggests that oxytocin activation in these areas influences several critical kidney functions:
• Renal hemodynamics: Oxytocin modulates blood flow through the kidneys, ensuring adequate perfusion while preventing excessive pressure that damages delicate filtering structures
• Systemic vascular resistance: By affecting blood vessel tone throughout the body, oxytocin helps maintain healthy blood pressure, reducing cardiovascular strain that accelerates kidney disease
• Glomerular filtration rate: Oxytocin may help preserve GFR the key measure of kidney function through pathways that overlap with but are distinct from vasopressin signaling
• Fluid balance and water handling: Studies show oxytocin can regulate renal water handling independently of vasopressin, particularly important in states of fluid imbalance commonly seen in CKD
By improving blood flow and ensuring adequate perfusion to nephrons (the kidney’s filtering units), oxytocin helps prevent ischemic injury a common contributor to kidney damage, scarring, and progressive loss of function.
Oxytocin Reduces Kidney Fibrosis and Scarring
Kidney fibrosis, the progressive scarring and hardening of kidney tissue, is a hallmark of advancing kidney disease regardless of the initial cause. Once fibrosis begins, it often progresses in a self-perpetuating cycle that’s difficult to halt with current therapies. Exciting animal studies suggest oxytocin interventions can significantly reduce tubulointerstitial fibrosis.
In research combining oxytocin administration with exercise training, investigators observed remarkable improvements:
• Significant reductions in molecular markers of fibrosis, including collagen deposition
• Improved renal tissue architecture with less scarring and better preservation of healthy nephrons
• Enhanced overall kidney pathology scores across multiple assessment parameters
• Better balance between pro-fibrotic factors and anti-fibrotic protective mechanisms
• Better preservation of kidney function over time compared to control groups
Oxytocin Protects Against Kidney Damage from Toxins and Injury
Multiple research studies demonstrate that oxytocin can alleviate kidney damage caused by various toxins, medications, and injury mechanisms:
• Cisplatin-induced nephrotoxicity: In animal models, oxytocin administration reduced kidney injury from this common chemotherapy drug, which frequently causes acute kidney damage in cancer patients
• Pyelonephritic injury: Oxytocin alleviated oxidative kidney damage in bacterial kidney infections through neutrophil-dependent mechanisms
• Bacterial endotoxin exposure: Oxytocin modulated neuroendocrine and cytokine responses to bacterial toxins, preventing excessive inflammatory responses
Social Connection and Kidney Health: The Oxytocin Link
Perhaps the most profound and clinically actionable finding is how social connection influences kidney health through oxytocin pathways. A fascinating study involving dialysis patients and animal-assisted therapy revealed this powerful connection in ways that challenge conventional thinking about kidney disease management.
Researchers studied end-stage kidney disease patients undergoing regular dialysis who participated in scheduled sessions with certified therapy dogs. Blood samples were collected to track oxytocin levels throughout the intervention period. The pattern observed was striking: initially, oxytocin levels showed a decrease, but then progressively increased across subsequent sessions with the animals.
This biphasic pattern suggests that dialysis patients may have atypical baseline oxytocin regulation that responds positively to consistent social stimulation. The findings indicate that positive social interactions, whether with animals or people, can normalise oxytocin signalling patterns in kidney disease patients, potentially conferring health benefits beyond emotional comfort.

Why Social Support Matters for Kidney Patients
The connection between social bonds and kidney health works through multiple oxytocin-mediated biological mechanisms that create measurable physiological changes:
• Meaningful social connection lowers cortisol and activates calming parasympathetic responses, reducing chronic stress that accelerates kidney disease progression
• Oxytocin release during social bonding supports healthy blood pressure regulation and improved heart rate variability
• Better vascular tone and reduced sympathetic nervous system activation improve blood flow to kidneys
• Oxytocin dampens inflammatory cytokine production, protecting kidney tissue from inflammatory damage
• Emotional support and accountability improve compliance with complex dietary restrictions and medication schedules
Practical Applications: Supporting Kidney Health Through Oxytocin Pathways
While we await further clinical research and potential therapeutic applications, you can support healthy oxytocin levels and kidney function today through evidence-based lifestyle approaches:
Dietary Strategies for Kidney Protection
• Focus on anti-inflammatory foods rich in omega-3 fatty acids like wild-caught fish, flaxseeds, and walnuts
• Include probiotic-rich fermented foods like yogurt, kefir, sauerkraut, and kimchi to support L. reuteri
• Consume prebiotic foods that feed beneficial bacteria: garlic, onions, leeks, asparagus, bananas, and oats
• Maintain appropriate protein intake while respecting any kidney-specific restrictions from your healthcare team
• Stay well-hydrated to support optimal kidney function, unless fluid restrictions apply

Lifestyle Practices for Kidney Health
• Prioritize meaningful social connections and community involvement, this is essential for health, not optional
• Practice regular stress-reduction techniques like meditation, yoga, tai chi, or progressive muscle relaxation
• Engage in moderate exercise appropriate for your health status, ideally including social activities
• Cultivate appropriate physical touch through massage, hugs with loved ones, or therapeutic bodywork
• Maintain regular sleep schedules and create a calming bedtime routine to support hormonal balance
• Consider animal-assisted activities or pet ownership if circumstances allow
• Join kidney disease support groups that combine social connection with practical guidance and shared experience
The Future of Oxytocin in Kidney Disease Treatment
The emerging research on oxytocin and kidney health reveals a fascinating mind-body connection that could transform how we approach chronic kidney disease prevention and treatment. Through its interaction with vasopressin pathways, direct effects on renal vascular tone and hemodynamics, potent anti-inflammatory properties, and anti-fibrotic actions, oxytocin appears to offer multiple protective mechanisms that work synergistically to preserve kidney function.
Perhaps most importantly, the connection between social support, positive relationships, and kidney health through oxytocin-mediated pathways highlights why psychosocial factors deserve equal consideration alongside medical treatments in kidney disease outcomes. Supportive relationships, community connections, and positive social experiences aren’t just emotionally beneficial; they may directly influence kidney function, inflammation, vascular health, and disease progression through measurable biological mechanisms.
For people living with chronic kidney disease, nurturing social connections, actively managing stress, supporting gut health through diet and probiotics, and fostering conditions for healthy oxytocin production may serve as valuable complementary approaches alongside conventional medical treatment. These lifestyle interventions are mainly safe, cost-effective, and accessible, yet they’re often overlooked in favor of purely pharmaceutical approaches.
As research continues to uncover the complex relationship between oxytocin and kidney function, we’re learning that the ‘love hormone’ may indeed have a profound healing role to play in kidney health reminding us that connection, both social and biological, forms the foundation of wellness. The future of kidney disease treatment may lie not only in advanced medications and procedures, but in rediscovering and supporting the biological wisdom that links love, connection, and physical health through powerful hormones like oxytocin.
Studies and Links
- Oxytocin alleviates oxidative renal injury in pyelonephritic rats via a neutrophil-dependent mechanism – ScienceDirect
- Oxytocin alleviates cisplatin-induced renal damage in rats – PubMed
- Hydrochlorothiazide combined with exercise training attenuates blood pressure variability and renal dysfunctions in an experimental model of hypertension and ovarian hormone deprivation
- Oxytocin alleviates the neuroendocrine and cytokine response to bacterial endotoxin in healthy men | American Journal of Physiology-Endocrinology and Metabolism | American Physiological Society
- Autoradiographic localization of vasopressin and oxytocin binding sites in rat kidney – ScienceDirect
- Animal Assisted Activities (AAAs) with the Dogs in a Dialysis Centre in Southern Italy: evaluation of serotonin and oxytocin values in involved patients | Research Square
- Can intranasal oxytocin reduce craving in automated addictive behaviours? A systematic review – PubMed
- Intranasal oxytocin increases neural responses to social reward in post-traumatic stress disorder – PubMed
- Effects of multiple-dose intranasal oxytocin administration on social responsiveness in children with autism: a randomized, placebo-controlled trial – PubMed
- The effect of oxytocin nasal spray on social interaction deficits observed in young children with autism: a randomized clinical crossover trial – PubMed
- What the vagus nerve and the hormone oxytocin tell the frontal lobe to do about stress | The Other Lobe of The Brain
- Oxytocin and the microbiome – ScienceDirect
- Research connecting gut bacteria and oxytocin provides a new mechanism for microbiome-promoted health benefits
- Research connecting gut bacteria and oxytocin provides a new mechanism for microbiome-promoted health benefits
- Frontiers | Role of oxytocin in bone