Discover the fundamental role electrons play in your health and learn science-backed strategies to optimize your body’s electrical balance for disease prevention and kidney protection.
Why Electrons Are the Missing Link in Your Health Journey
Most people think about health in terms of diet, exercise, and medications, but there’s a fundamental layer that’s often overlooked: your body’s electrical system. Electrons, the tiny negatively charged particles that orbit atoms, are not just abstract concepts from chemistry class; they’re the driving force behind every biological process in your body.
As Nobel Prize winner Albert Szent-Györgyi famously said, “Life is nothing but an electron looking for a place to rest.” This profound statement reveals a truth that modern medicine is only beginning to fully appreciate: your health is fundamentally dependent on the proper flow and balance of electrons throughout your body.
The ElectronHealth Connection: By the Numbers
- Every cell in your body depends on electron transfer for energy production
- Mitochondrial dysfunction (impaired electron flow) is linked to over 80% of chronic diseases
- Oxidative stress from electron imbalance contributes to aging and disease progression
- Grounding therapy can reduce inflammation by up to 50% through electron transfer from Earth
For those dealing with chronic kidney disease, understanding electron balance becomes even more critical, as kidney function is intimately connected to your body’s ability to maintain proper electrical and chemical equilibrium.
Understanding Your Body’s Electrical System: Electrons in Action
The Fundamental Role of Electrons in Human Biology
Electrons are far more than just components of atoms, they’re the currency of life itself. Every breath you take, every heartbeat, every thought you think depends on the precise orchestration of electron movement throughout your body. These subatomic particles serve as the building blocks of all biological processes, making their proper function essential for optimal health.
Key Functions of Electrons in Your Body:
- Energy metabolism through the electron transport chain
- Nerve transmission enabling communication between brain and body
- Antioxidant protection against cellular damage
- Immune system regulation and pathogen defense
- Detoxification processes in liver and kidneys
- DNA repair mechanisms preventing genetic mutations
Without a constant, well-regulated flow of electrons, even the most basic physiological functions would cease. This makes electron balance not just crucial for health it makes it absolutely essential for survival.
Cellular Respiration: Your Body’s Energy Factory
The human body’s primary energy production occurs through cellular respiration, a sophisticated process that takes place in the mitochondria, often called the “powerhouses of the cell.” This process exemplifies the critical importance of electron flow in maintaining health and preventing chronic disease.
The Three-Stage Energy Production Process:
Stage 1: Glycolysis – The Initial Electron Harvest During glycolysis, a single glucose molecule is systematically broken down into two pyruvate molecules. This process generates NADH (nicotinamide adenine dinucleotide) and a modest amount of ATP. The key here is the transfer of electrons from glucose intermediates to NAD+, forming the electron carrier NADH. This electron capture is essential for the subsequent energy production stages.
Stage 2: Krebs Cycle – Electron Amplification In the mitochondrial matrix, pyruvate undergoes further oxidation through the Krebs cycle (also known as the citric acid cycle). This process produces multiple electron carriers: NADH and FADH2 (flavin adenine dinucleotide). These molecules act as electron shuttles, capturing high-energy electrons and transporting them to the final stage of energy production.
Stage 3: Oxidative Phosphorylation – The Electron Highway This is where the magic happens. Electrons are transferred through a series of protein complexes embedded in the inner mitochondrial membrane the electron transport chain. As electrons move through these complexes, they release energy that pumps protons across the membrane, creating an electrochemical gradient. This gradient drives ATP synthase, the molecular machine that produces ATP, your body’s primary energy currency.
When Electron Flow Goes Wrong: The Chronic Disease Connection
Chronic diseases often stem from defects in this electron transport chain, fundamentally impairing the cell’s ability to produce adequate ATP. When electron flow is disrupted, cells experience energy deficits that cascade into organ dysfunction and, ultimately, disease states.
Common Causes of Electron Transport Chain Dysfunction:
- Mitochondrial DNA mutations inherited or acquired over time
- Environmental toxins that damage mitochondrial components
- Nutrient deficiencies affecting electron transport proteins
- Oxidative stress overwhelming protective mechanisms
- Age-related deterioration of mitochondrial function
- Chronic inflammation impairing cellular energy production
This dysfunction is particularly relevant for kidney health, as kidneys are among the most energy-demanding organs in the body, requiring efficient electron flow to perform their complex filtration and regulatory functions.
The Double-Edged Sword: Redox Reactions and Reactive Oxygen Species
Understanding Redox: The Biological Game of Pass the Electron
Redox reactions, short for reduction-oxidation reactions, can be understood as a sophisticated game of “pass the electron.” In this biological game, one molecule gains an electron (reduction) while another loses an electron (oxidation). This electron exchange is continuous and essential, fuelling everything from muscle contractions to complex cognitive processes.
Your Body’s Defense Network: Antioxidants as Electron Donors
The Antioxidant Arsenal: Your Cellular Protective Force
Antioxidants serve as your body’s primary defense against oxidative damage. These remarkable molecules have the unique ability to donate electrons to unstable ROS without becoming dangerous free radicals themselves. This electron-donating capacity makes them essential for maintaining cellular health and preventing chronic disease.
Primary Antioxidant Functions:
- Free radical neutralization through electron donation
- DNA protection preventing genetic mutations
- Mitochondrial preservation maintaining energy production capacity
- Immune cell support optimizing defense mechanisms
- Inflammatory regulation preventing excessive tissue damage
- Recovery acceleration after exercise, stress, or illness
Key Antioxidant Categories:
Enzymatic Antioxidants:
- Superoxide dismutase (SOD): Converts superoxide radicals to hydrogen peroxide
- Catalase: Breaks down hydrogen peroxide to water and oxygen
- Glutathione peroxidase: Reduces lipid peroxides and hydrogen peroxide
Non-Enzymatic Antioxidants:
- Vitamin C: Water-soluble electron donor, crucial for immune function
- Vitamin E: Fat-soluble protector of cell membranes
- Glutathione: The “master antioxidant” produced by your cells
- Coenzyme Q10: Essential for mitochondrial electron transport
- Polyphenols: Plant compounds with powerful antioxidant properties
The Antioxidant-Kidney Health Connection
For individuals with chronic kidney disease, antioxidant status becomes particularly crucial. Kidneys are highly susceptible to oxidative damage due to their:
- High metabolic activity requiring constant energy production
- Exposure to toxins during filtration processes
- Rich blood supply increasing ROS exposure
- Limited regenerative capacity making damage particularly concerning
Research consistently shows that CKD patients have significantly reduced antioxidant capacity and elevated oxidative stress markers, creating a vicious cycle where kidney damage accelerates further oxidative injury.
Grounding: Harnessing Earth’s Electron Supply for Health
The Earth as Your Natural Antioxidant Source
Modern life has disconnected us from one of nature’s most abundant sources of electrons: the Earth itself. The planet’s surface maintains a negative electrical charge, providing an essentially unlimited supply of free electrons. Research suggests that this disconnection from Earth’s electron supply may be a significant contributor to chronic inflammation and disease.
The Science of Grounding: Grounding, also called earthing, involves direct physical contact with the Earth’s surface, allowing the transfer of electrons from the ground into your body. This can be achieved through:
- Walking barefoot on grass, sand, or soil
- Swimming in natural bodies of water
- Using grounding systems that connect you to Earth’s electrical field indoors
- Gardening with direct soil contact
Documented Health Benefits of Grounding
Research has documented numerous physiological improvements from regular grounding practice:
Inflammation Reduction: Studies show that grounding can reduce key inflammatory markers, including C-reactive protein and white blood cell counts. This anti-inflammatory effect appears to result from the neutralization of free radicals by Earth’s electrons.
Sleep Quality Improvement: Grounding has been shown to normalize circadian cortisol rhythms, leading to better sleep quality and reduced nighttime stress hormone levels.
Pain Management: Clinical trials demonstrate significant pain reduction in individuals practicing regular grounding, likely due to the anti-inflammatory effects of electron transfer.
Cardiovascular Benefits: Grounding may improve heart rate variability and reduce blood viscosity, potentially benefiting cardiovascular health.
Stress Reduction: Measurements of autonomic nervous system activity show that grounding promotes parasympathetic (relaxation) nervous system activation while reducing sympathetic (stress) responses.
For kidney patients, these benefits are particularly valuable, as chronic inflammation, poor sleep, and cardiovascular stress all contribute to disease progression.
Electrons and Cardiovascular Disease: The Nitric Oxide Connection
The Critical Role of Nitric Oxide in Vascular Health
Cardiovascular health is intimately connected to electron balance through the nitric oxide (NO) pathway. Nitric oxide is a crucial signaling molecule that helps blood vessels relax, maintain proper blood pressure, and resist atherosclerotic changes.
Nitric Oxide’s Protective Functions:
- Vasodilation: Relaxes blood vessel walls, reducing blood pressure
- Anti-inflammatory effects: Reduces vascular inflammation
- Antithrombotic properties: Prevents dangerous blood clot formation
- Endothelial protection: Maintains healthy blood vessel lining
The Electron Connection: Nitric oxide is highly redox-sensitive, meaning its function depends heavily on the local electron environment. When adequate antioxidant electrons are available, NO remains stable and active. However, during oxidative stress, NO reacts with superoxide radicals to form peroxynitrite, a highly damaging compound.
The Cardiovascular-Kidney Disease Link
This cardiovascular-electron connection has profound implications for kidney health:
- Hypertension from impaired NO function damages kidney blood vessels
- Atherosclerosis reduces blood flow to kidneys
- Endothelial dysfunction impairs kidney filtration capacity
- Chronic inflammation accelerates both cardiovascular and kidney disease
Understanding these connections helps explain why cardiovascular disease and kidney disease so often occur together, and why interventions that improve electron balance often benefit both systems.
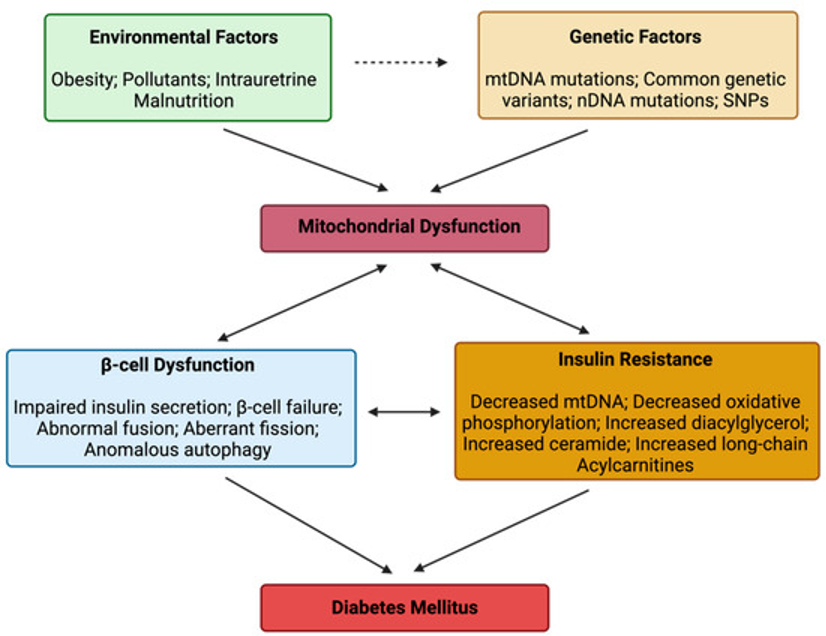
The Mitochondrial Traffic Jam
Type 2 diabetes and metabolic syndrome provide perfect examples of how disrupted electron flow leads to chronic disease. In these conditions, mitochondria become overwhelmed by excessive glucose and fatty acids, creating what researchers describe as a “mitochondrial traffic jam.”
The Pathological Process:
- Nutrient Overload: Excessive glucose and fatty acids flood mitochondria
- Electron Transport Saturation: The electron transport chain becomes overwhelmed
- Premature Electron Leakage: Electrons “spill out” before completing the transport process
- Excessive ROS Production: Leaked electrons react with oxygen, creating harmful free radicals
- Cellular Damage: ROS damage mitochondrial components, perpetuating the dysfunction
Image via Mitochondrial Dysfunction in Diabetes: Shedding Light on a Widespread Oversight
This mitochondrial dysfunction triggers multiple pathological processes:
Insulin Resistance: Damaged mitochondria cannot efficiently process glucose, leading to cellular insulin resistance. Muscle and liver cells become less responsive to insulin signals, requiring higher insulin levels to achieve glucose uptake.
Beta Cell Dysfunction: Pancreatic beta cells, which produce insulin, are particularly vulnerable to oxidative damage due to their low antioxidant capacity. Chronic ROS exposure leads to progressive beta cell death and diabetes progression.
Systemic Inflammation: Mitochondrial dysfunction activates inflammatory pathways, creating chronic low-grade inflammation that further impairs insulin sensitivity and promotes disease progression.
Endothelial Dysfunction: Impaired electron flow compromises nitric oxide production, leading to vascular dysfunction that contributes to diabetic complications, including kidney disease.
The Diabetes-Kidney Disease Connection
Diabetic kidney disease (diabetic nephropathy) represents one of the most serious complications of diabetes and is directly linked to mitochondrial dysfunction:
- High glucose levels create oxidative stress in kidney cells
- Advanced glycation end products damage kidney proteins
- Inflammatory processes promote kidney fibrosis
- Vascular dysfunction impairs kidney blood flow
This explains why diabetes is the leading cause of chronic kidney disease in developed countries and why interventions that improve mitochondrial function often benefit both diabetes control and kidney health.
The Rising Tide: Why Chronic Kidney Disease Is Becoming More Common
The Perfect Storm of Modern Risk Factors
Chronic kidney disease rates have skyrocketed in recent decades, and electron balance disruption plays a central role in this epidemic. Multiple factors in modern life conspire to impair electron flow and increase oxidative stress:
Dietary Factors:
- Processed foods high in advanced glycation end products
- Excessive sugar consumption overwhelming mitochondrial capacity
- Trans fats damaging mitochondrial membranes
- Nutrient depletion from soil degradation and food processing
Lifestyle Factors:
- Sedentary behavior reducing mitochondrial biogenesis
- Chronic stress depleting antioxidant reserves
- Poor sleep quality impairing cellular repair processes
- Environmental toxin exposure damaging mitochondrial DNA
Medical Factors:
- Medication side effects particularly from certain antibiotics and pain medications
- Frequent imaging procedures with contrast agents
- Chronic inflammatory conditions creating persistent oxidative stress
The Interconnected Web of Chronic Disease
The electron dysfunction underlying these risk factors creates a web of interconnected health problems:
- Diabetes and obesity create mitochondrial overload
- Hypertension damages kidney blood vessels through oxidative mechanisms
- Cardiovascular disease reduces kidney blood flow
- Chronic inflammation accelerates disease progression across all systems
This interconnection explains why kidney disease rarely occurs in isolation; it typically develops alongside other chronic conditions, all sharing the common thread of electron transport dysfunction.
Evidence-Based Interventions to Optimize Electron Flow
Nutritional Strategies for Electron Balance
Antioxidant Powerhouses:
- Vitamin C: 500-1000mg daily for immune support and electron donation
- Vitamin E: 400-800 IU daily for membrane protection (consult healthcare provider for kidney patients)
- Coenzyme Q10: 100-200mg daily for mitochondrial support
- Alpha-lipoic acid: 300-600mg daily for versatile antioxidant protection
- Polyphenol-rich foods: Berries, dark chocolate, green tea, and colorful vegetables
Mitochondrial Support Nutrients:
- Magnesium: 300-400mg daily for enzyme cofactor functions
- B-complex vitamins: Essential for energy metabolism pathways
- Omega-3 fatty acids: 1-2g daily for membrane health and inflammation control
- N-acetylcysteine: 600-1200mg daily for glutathione production (particularly important for kidney patients)
Exercise: The Mitochondrial Multiplier
Regular physical activity represents one of the most powerful interventions for improving electron flow and mitochondrial function:
Mitochondrial Benefits of Exercise:
- Increased mitochondrial biogenesis: Exercise stimulates the creation of new mitochondria
- Improved electron transport efficiency: Regular activity optimizes the electron transport chain
- Enhanced antioxidant enzyme production: Exercise upregulates natural antioxidant systems
- Better glucose metabolism: Physical activity improves cellular insulin sensitivity
Exercise Recommendations for Kidney Health:
- Moderate aerobic exercise: 150 minutes per week of brisk walking or similar activity
- Resistance training: 2-3 sessions per week to maintain muscle mass and metabolic function
- High-intensity interval training: Short bursts of intense activity (with medical clearance)
- Flexibility and balance work: Yoga or tai chi for stress reduction and body awareness
Intermittent fasting has emerged as a powerful tool for improving mitochondrial function and electron flow:
Metabolic Benefits:
- Mitochondrial autophagy: Fasting triggers the removal of damaged mitochondria
- Ketone production: Alternative fuel source that bypasses glycolytic dysfunction
- Improved insulin sensitivity: Reduced glucose load allows mitochondrial recovery
- Activation of cellular repair pathways: Fasting stimulates various protective mechanisms
Considerations for Kidney Patients: Intermittent fasting should be approached cautiously in CKD patients and only under medical supervision, as kidney function affects the body’s ability to maintain electrolyte and acid-base balance during fasting periods.
Environmental and Lifestyle Interventions
Grounding Practices:
- Daily barefoot contact with Earth for 20-30 minutes
- Indoor grounding systems for consistent electron access
- Natural water swimming when possible
- Gardening with direct soil contact
Light Therapy:
- Morning sunlight exposure for circadian rhythm optimization
- Red light therapy for mitochondrial stimulation
- Blue light avoidance in evening hours to protect sleep quality
Stress Management:
- Meditation practices to reduce oxidative stress
- Deep breathing exercises to activate parasympathetic nervous system
- Regular nature exposure for psychological and physiological benefits
- Social connection to buffer against chronic stress
Advanced Strategies for Kidney Patients: Optimizing Electron Flow
Kidney-Specific Electron Support
For individuals with chronic kidney disease, optimizing electron flow requires special considerations:
Kidney-Safe Electron Enhancement:
- Targeted polyphenol intake from berries, pomegranates, and green tea
- Optimized magnesium levels within kidney-safe ranges
- Careful potassium management balancing antioxidant foods with kidney function
- Phosphorus-conscious antioxidant choices to prevent mineral bone disease
Monitoring and Assessment
Laboratory Markers for Electron Status:
- Glutathione levels: Direct measure of primary cellular antioxidant
- Oxidative stress markers: Including malondialdehyde and 8-OHdG
- Inflammatory markers: C-reactive protein, IL-6, and TNF-alpha
- Mitochondrial function tests: Specialized assessments of cellular energy production
Functional Assessments:
- Energy levels and fatigue patterns: Subjective measures of mitochondrial function
- Exercise tolerance: Objective measure of cellular energy capacity
- Sleep quality and recovery: Indicators of cellular repair processes
- Cognitive function: Brain energy metabolism assessment
Conclusion: Reclaiming Your Electrical Health
Understanding the fundamental role of electrons in health opens up entirely new possibilities for preventing and managing chronic disease, particularly chronic kidney disease. By recognizing that your body is fundamentally an electrical system that depends on proper electron flow, you can take targeted actions to optimize this crucial aspect of your physiology.
The interventions discussed in this guide, from antioxidant nutrition to grounding practices, from exercise protocols to stress management, all work by supporting your body’s electron balance and mitochondrial function. For individuals with kidney disease, this understanding becomes particularly crucial, as kidney function is intimately connected to your body’s electrical and chemical equilibrium.
The rising rates of chronic kidney disease in our modern world are not inevitable. By addressing the underlying electron imbalances that contribute to disease development and progression, we can work toward not just managing kidney disease, but potentially preventing it entirely.
This comprehensive guide provides educational information and should complement, not replace, professional medical advice. Always consult with your healthcare provider before making significant changes to your health regimen, particularly if you have chronic kidney disease.
References